Bacterial infections (4)
- 1. BACTERIAL DISEASES Prepared by: Dr. Rea Corpuz
- 2. Bacterial Diseases (1) Syphillis (2) Tuberculosis (3) Leprosy (4) Actinomycosis (5) Cancrum Oris (NOMA) (6) Gonorrhea
- 3. (1) Syphillis sexually transmitted disease caused by spirochete Treponema Pallidum acquired by sexual contact with a partner with active lesions by: transfusion of infected blood transplacental inoculation of fetus by infected mother
- 4. (1) Syphillis Pathogenesis when disease is spread through direct contact a hard ulcer, or chancre forms at site of spirochete later there is development of painless, non-suppurative regional lymphadenopathy
- 5. (1) Syphillis Pathogenesis chancre heals spontaneously after several weeks without treatment, leaving patient with no apparent signs of disease
- 6. (1) Syphillis Pathogenesis after a latent period of several weeks, secondary syphilis develops • patients infected via transfusion bypass primary stage & begin with secondary syphilis
- 7. (1) Syphillis Pathogenesis secondary syphilis • fever • flulike symptoms • mucucutaneous lesions • lymphadenopathy • stage resolves spontaneously, • patient enters latency period
- 8. (1) Syphillis Clinical Features Primary Phase Secondary Phase Tertiary Phase Congenital Phase
- 9. (1) Syphillis Clinical Features Primary Phase • does not produce exudate • location is usually on genitalia • lesions heals without therapy in 3-12 weeks, with little or no scarring
- 10. (1) Syphillis Clinical Features Primary Phase • Chancre, a chronic ulcer at site of infection
- 11. (1) Syphillis Clinical Features Secondary Phase • if left untreated, begins about 2-10 weeks • spirochetes are now disseminated widely • inflammatory lessions may occur in any organ during this phase
- 12. (1) Syphillis Clinical Features Secondary Phase • Oral mucous patches • condyloma latum • maculopapular rash
- 13. (1) Syphillis Clinical Features Tertiary Phase • manifestations take many years to appear & can be profound • there is predilection for cardiovascular system + CNS
- 14. (1) Syphillis Clinical Features Tertiary Phase • Gummas (destructive ulcers) • central nervous system • cardiovascular diseases
- 15. (1) Syphillis Clinical Features Congenital Form • abnormal shape of molars/ incisors • deafness • ocular keratitis • skeletal defects
- 16. (1) Syphillis Treatment drug of choice for treating all stages of syphillis is penicillin Treponema Pallidum is sensitive to antibiotics such as: • Penicillin • Erythromycin • Tetracycline
- 17. (2) Tuberculosis infects about 1/3 of world’s population kills approximately 3 million people per year most important cause of death in the world
- 18. (2) Tuberculosis caused by aerobic, non-spore forming bacillus Mycobacterium Tuberculosis has thick, waxy coat does not react with Gram stains
- 19. (2) Tuberculosis Pathogenesis spread is through small airborne droplets • carry organism to pulmonary air spaces
- 20. (2) Tuberculosis Clinical Features skin testing + chest radiograph • provide only indicators of infection
- 21. (2) Tuberculosis Clinical Features in reactivated disease, • low-grade signs + symptoms of fever • night sweats • malaise • weight loss
- 22. (2) Tuberculosis Clinical Features with progression, • cough • hemoptysis • chest pain (pleural involvement)
- 23. (2) Tuberculosis Clinical Features oral manifestations • follow implantation of M. tuberculosis from infected sputum may appear on any mucosal surface • tongue + palate are favored locations
- 24. (2) Tuberculosis Clinical Features oral manifestations • typical lesion is indurated chronic, nonhealing ulcer that is usually painful • bony involvement of maxilla + mandible may produce tuberculosis osteomyelitis
- 25. (2) Tuberculosis Treatment First line drugs likely to used fro treatment of TB include • isoniazid • rifampin • pyrazinamide • exambuthol
- 26. (2) Tuberculosis Treatment drug combinations are often used in 6, 9, or 12 month treatment regimens may be extended as long as 2 years.
- 27. (2) Tuberculosis Treatment Bacille Calmette Guerin (BCG) vaccine is effective in controlling childhood TB, but loses efficacy in adulthood
- 28. (3) Leprosy also known as Hansen’s disease chronic infectious disease caused by acid-fast bacillus, Mycobacterium leprae moderately contagious
- 29. (3) Leprosy transmission of disease requires frequent direct contact with an infected individual for a long period inoculation through respiratory tract is also believed to be a potential mode of transmission
- 30. (3) Leprosy Clinical Features there is clinical spectrum of disease that ranges from a limited form (tuberculoid leprosy) to a generalized form (lepromatous leprosy) latter has a more seriously damaging course
- 31. (3) Leprosy Clinical Features skin + peripheral nerves are affected organism grows best in temperatures less than core body temp of 37C
- 32. (3) Leprosy Clinical Features cutaneous lesions appear as erythematous plaques or nodules • represents granulomatous response to organism similar lesions may occur intraorally or intranasally
- 33. (3) Leprosy Clinical Features in time, severe maxillofacial deformaties can appear • producing classic destruction of anterior maxilla • facies leprosa
- 34. (3) Leprosy Treatment chemotherapeutic approach in which, several drugs are used for protracted period, typically years
- 35. (3) Leprosy Treatment commonly used drugs: • dapsone • rifampin • clofazimine • minocycline • teratogen thalidomide useful to manage complications of leprosy therapy
- 36. (4) Actinomycosis chronic bacterial disease exhibits some clinical + microscopic features that are fungilike caused by Actinomyces israelii an anaerobic or microaerophilic gram-positive bacterium not regarded as contagious because infection cannot be transmitted from one individual to another
- 37. (4) Actinomycosis infections usually appear after trauma surgery previous infection
- 38. (4) Actinomycosis Clinical Features most infections are seen: • thorax usually preceded • abdomen by trauma or direct • head + neck extension of contagious infectiom
- 39. (4) Actinomycosis Clinical Features when it occurs in head + neck • condition is usually designated cervicofacial actinomycosis swelling of mandible skin lesion are indurated having woody hard consistency results to osteomyelitis that may drain through gingiva
- 40. (4) Actinomycosis Radiographic Feature radiolucency irregular + ill-defined margins
- 41. (4) Actinomycosis Treatment Long-term, high-dose penicillin For sever cases, intravenous penicillin followed by oral penicillin Tetracycline + Erythromycin can be used
- 42. (4) Actinomycosis Treatment drainage of abscess surgical excison of scar + sinus tracts • to enhance penetration of antibiotics
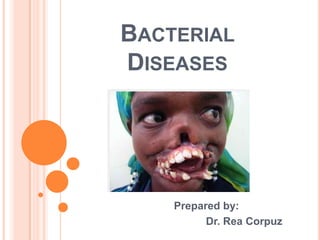
- 43. (5) Cancrum Oris (Noma) also known as gangrenous stomatitis devastating disease of malnourished children destructive process of orofacial tissues
- 44. (5) Cancrum Oris (Noma) results from oral contamination by heavy infestation of Bacteroidaceae particularly Fusobacterium necrophorum
- 45. (5) Cancrum Oris (Noma) consortium of other microorganisms: Borrelia vincentii Staphylococcus aureus Prevotella intermedia
- 46. (5) Cancrum Oris (Noma) these opportunistic pathogens invade oral tissues whose defense are weakened by: malnutrition acute necrotizing gingivitis debilitating conditions
- 47. (5) Cancrum Oris (Noma) these opportunistic pathogens invade oral tissues whose defense are weakened by: trauma other oral mucosal ulcers
- 48. (5) Cancrum Oris (Noma) Clinical Features typically affects children related disorder, noma neonatorum, oocurs in low- birth-weight infants who suffer from debilitating diseases
- 49. (5) Cancrum Oris (Noma) Clinical Features initial lesion is a painful ulceration usually gingiva or buccal mucosa spreads rapidly + eventually becomes necrotic
- 50. (5) Cancrum Oris (Noma) Clinical Features denudation of involved bone may follow leading to necrosis + sequestration
- 51. (5) Cancrum Oris (Noma) Clinical Features teeth in affected area may become loose + exfoliate penetration of organisms into • cheek • lip • palate
- 52. (5) Cancrum Oris (Noma) Treatment fluids electrolytes general nutrition are restored along with antibiotics • clindamycin • piperacillin • aminoglycoside gentamicin
- 53. (5) Cancrum Oris (Noma) Treatment fluids electrolytes general nutrition are restored along with antibiotics • clindamycin • piperacillin • aminoglycoside gentamicin
- 54. (5) Cancrum Oris (Noma) Treatment debridement of necrotic tissue may also be beneficial if destruction is extensive
- 55. (6) Gonorrhea one of the most prevalent bacterial disease in humans caused by gram-negative diplococcus Neisseria gonorrhoeae infects columnar epithelium of • lower genital tract • rectum • pharynx • eyes
- 56. (6) Gonorrhea transmitted by direct sexual contact with an infected partner short incubation period of less than 7 days absence of symptoms in many individuals, especially females
- 57. (6) Gonorrhea genital infections may be transmitted to oral or pharyngeal mucous membranes through orogenital contact transmission from an infected patient to dental personnel is regarded as highly unlikely
- 58. (6) Gonorrhea organism is very sensitive to drying requires break in skin or mucosa to establish an infection gloves provide protective eyewear adequate protection mask from accidental transmission
- 59. (6) Gonorrhea Clinical Features no specific clinical signs have been consistently associated with oral gonorrhea multiple ulcerations generalized erythema
- 60. (6) Gonorrhea Clinical Features in the more common pharyngeal gonococcal infection, presenting signs are usally • general erythema • associated ulcers • cervical lymphadenopathy
- 61. (6) Gonorrhea Clinical Features chief complaint may be sore throat, although many patients are asymptomatic
- 62. (6) Gonorrhea Treatment uncomplicated gonorrhea responds to single dose of appropriately selected antibiotic
- 63. References: Books Neville, et. al: Oral and Maxillofacial Pathology 3rd Edition • (pages 24-32)
