Presentation1.pptx, ultrasound examination of the knee joint.
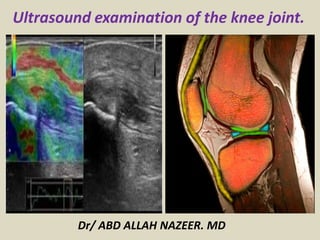
- 1. Dr/ ABD ALLAH NAZEER. MD Ultrasound examination of the knee joint.
- 2. ULTRASOUND OF THE KNEE – Normal. Transverse scan plane for the quadriceps Transverse suprapatella region: •RF: Rectus Femoris •VI: Vastus intermedius •VL: Vastus Lateralis •VM: Vastus Medialis
- 3. Suprapatellar scan plane. Longitudinal suprapatella region showing the suprapatella bursa and quadriceps tendon.
- 5. Infrapatellar scan plane. The infrapatellar tendon. Also called the patella ligament.
- 6. The insertion of the infrapatellar tendon onto the tibial tuberosity. Note: The normal physiological amount of fluid along the underside of the tendon. Transverse Infrapatellar tendon. Note how wide it is, to then have an understanding of the area you need to examine in longitudinal.
- 7. Pes anserine scan plane. The Pes Anserine bursa and tendon insertion are medial to the Infrapatellar tendon on the tibia, adjacent to the MCL insertion. Remember the Pes Anserine tendons as (sargent) SGT: Sartorius, Gracilis and semi-Tendinosis.
- 8. Medial knee joint scan plane. The medial collateral ligament (green) directly overlying the medial meniscus (purple).
- 9. Lateral knee joint scan plane. Assess the Lateral collateral ligament, Ilio-Tibial band insertion and peripheral margins of the lateral meniscus. Unlike the medial side, the LCL is separated from the meniscus by a thin issue plane.
- 10. Ilio-Tibial Band. Rotate the probe off the LCL with the toe of the probe angled slightly posteriorly.
- 11. Popliteal fossa scan plane. Medial aspect of the popliteal fossa showing the semimembranosis/gastrocnemius plane.
- 12. Ultrasound of the Popliteal vein and artery in transverse. Without and with compression to exclude DVT. Confirm both arterial and venous flow and exclude a popliteal artery aneurysm
- 26. ROLE OF ULTRASOUND Ultrasound is essentially used for the external structures of the knee. Ultrasound is a valuable diagnostic tool in assessing the following indications; Muscular, tendinous and ligamentous damage (chronic and acute) Bursitis Joint effusion Popliteal vascular pathology Haematomas Masses such as Baker’s cysts, lipomas Classification of a mass e.g solid, cystic, mixed Post surgical complications e.g abscess, edema Guidance of injection, aspiration or biopsy Relationship of normal anatomy and pathology to each other Some boney pathology LIMITATIONS It is recognised that ultrasound offers little or no diagnostic information for internal structures such as the cruciate ligaments. Ultrasound is complementary with other modalities, including plain X-ray, CT, MRI and arthroscopy. EQUIPMENT SELECTION AND TECHNIQUE Use of a high resolution probe (7-15MHZ) is essential when assessing the superficial structures of the knee. Careful scanning technique to avoid anisotropy (and possible misdiagnosis) Beam steering or compounding can help to overcome anisotropy in linear structures such as tendons. Good colour / power / Doppler capabilities when assessing vessels or vascularity of a structure. Be prepared to change frequency output of probe (or probes) to adequately assess both superficial and deeper structures.
- 27. SCANNING TECHNIQUE POSTERIOR FOSSA Patient prone on bed, knee flexed slightly with a pad under the ankle for support. Survey the entire fossa to identify the normal anatomy, including; Popliteal artery and vein (patency. aneurysm, thrombosis) Posterior joint (joint effusion) Medial popliteal fossa [ bursa between semi-membranosis tendon and medial gastrocnemius muscle] (Baker’s cyst) Document the normal anatomy and any pathology found, including measurements and vascularity if indicated. ANTERIOR KNEE Patient lies supine on bed with knee flexed 20 - 30 degrees. Alternatively patient may sit on the side of a raised bed with foot resting on Sonographers knee for support. Identify the normal anatomy, including: Quadriceps tendon (tears, M/T junction, tendonitis) Suprapatella bursa (bursitis-simple/complex, synovial thickening, loose bodies) Patella (gross changes e.g erosion, bipartite, fracture) Patella tendon (tears, tendonitis, insertion enthesopathy) Infrapatellar bursa (tendinosis, tears, bursitis, fat pad changes) Infero-Medial - Pes anserine bursa. LATERAL AND MEDIAL KNEE May be scanned as above. Assess the medial and Lateral Collateral ligaments and meniscal margins. Joint lines (ligament tears or thickening, meniscal bulging/cysts, joint effusion, gross bony changes).
- 28. BASIC IMAGING A knee series should include the following minimum images; Quadriceps tendon - long, trans +/- MT junction Suprapatellar bursa Pre patellar - long Patella tendon - long, trans, insertion onto tibial tuberosity Medial meniscus and MCL Lateral Meniscus and LCL Popliteal artery and vein to demonstrate patency Medial popliteal fossa Document the normal anatomy and any pathology found, including measurements and vascularity if indicated.
- 29. “Jumper’s knee” or patellar tendinosis is a common condition affecting athletes with an incidence in this subpopulation of 13% to 20%. It is particularly prevalent in sports involving jumping and heavy landing, rapid acceleration or deceleration and kicking, such as basketball, volleyball, soccer, tennis, long jump and high jump. It has a tendency to become chronic and, in elite athletes, the incidence of having to retire from their sport is as high as 53%. Imaging: Both ultrasound and MRI have been described for the diagnosis of patellar tendinosis. Ultrasound has traditionally been used to image tendons and reveals consistent findings in patellar tendinitis. The tendon reveals an area of hypoechoic signal change and increased thickness corresponding to the area of clinical tenderness. Colour Doppler examination is a useful adjunct as it has been shown to identify vascularity and neovessels in the area of structural change.
- 30. Patellar tendinopathy. Longitudinal ultrasound scan along the anterior aspect of the knee joint shows thickened tendon .
- 31. Patellar tendinopathy with thickened distal patellar tendon longitudinal with increased vascularity.
- 32. Tendinosis of the distal patellar tendon insertion with neovascularity and slightly thickened bursa.
- 33. US show partial thickness tear of the quadriceps tendon.
- 34. A sagittal image of the affected left knee demonstrates the ruptured quadriceps tendon (T) attached to the superior pole of the patella (P). Note the loss of linear fibers of the tendon, which is filled in by an effusion (*) anterior to the distal femur (F)
- 35. The prepatellar bursa is a superficial bursa with a thin synovial lining located between the skin and the patella. Normally, it does not communicate with the joint space and contains a minimal amount of fluid; however, inflammation of the Prepatellar bursa results in marked increase of fluid within its space. Prepatellar bursitis is often caused by pressure from constant kneeling. Plumbers, roofers, carpet layers, coal miners, and gardeners are at greater risk for developing the condition. A direct blow to the front of knee can also cause prepatellar bursitis. Athletes who participate in sports in which direct blows or falls on the knee are common, such as football, wrestling, or basketball, are at greater risk for the condition. Musculoskeletal ultrasound is emerging as a viable imaging modality to assess the knee joint. Advantages include its ease of availability, economic savings compared to MRI, ability to easily compare abnormalities to the contralateral side, demonstration of fibrillar microanatomy of tendons, ligaments, and muscles, and the ability to compress and dynamically assess structures. Musculoskeletal ultrasound can be utilized to distinguish difficult cases of joint effusion from that of bursal swelling.
- 36. Prepatellar bursitis. Longitudinal midline ultrasound scan shows distension of the Prepatellar bursa with a sonolucent fluid collection with coarse internal echoes.
- 37. Ultrasound prepatellar bursitis (a) and a septal pattern (b)
- 38. Prepatellar bursitis with thickened hypoechoic bursa anterior of the patellar tendon.
- 40. Osgood-Schlatter disease (OSD) is a chronic fatigue injury due to repeated microtrauma to involving the patellar ligament insertion onto the tibial tuberosity. Ultrasound Ultrasound examination of the patellar tendon can depict the same anatomic abnormalities as can plain radiographs, CT scans, and magnetic resonance images. The sonographic appearances in Osgood-Schlatter disease include: swelling of the unossified cartilage and overlying soft tissues fragmentation, and irregularity of the ossification center with reduced internal echogenicity thickening of the distal patellar tendon infrapatellar bursitis.
- 41. Osgood Schlatter on both sides with cartilage swelling and fragmentation of the apophysis.
- 42. Osgood Schlatter disease with irregular apophysis and infrapatellar bursitis and tendinosis
- 43. Osgood schlatter disease with irregular apophysis and infrapatellar bursitis and tendinosis with a hypervascularized inhomogeneous patellar tendon
- 44. Osgood schlatter disease with cartilage swelling and irregular apophysis and thickened hypervascularized inhomogeneous patellar tendon.
- 45. Medial collateral ligament (MCL) and lateral collateral ligament (LCL) injuries of the knee are common. In fact, injury to the MCL is the most common ligamentous knee injury. The MCL and LCL provide restraint to valgus and varus angulation of the knee, respectively. The MCL has superficial and deep components. The superficial MCL fibers attach proximally to the medial femoral epicondyle and distally to the medial aspect of the tibia, approximately 4 cm distal to the joint line. The deep MCL fibers originate from the medial joint capsule and are attached to the medial meniscus. The LCL is part of a complex of ligaments collectively named the posterolateral corner (PC). The structures in the PC include the LCL, the popliteofibular ligament, the popliteus ligament, the arcuate ligament, the short lateral ligament, and the posterolateral joint capsule. The LCL is separated from the lateral meniscus by a fat pad. All injured collateral ligament structures were thickened and heterogeneously hypoechoic. Ultrasonography is useful in evaluating isolated collateral ligament injuries and in predicting patient outcome on the basis of the location of the collateral ligament injuries.
- 46. Partial thickness tear of the medial collateral ligament with an inhomogeneous thickened ligament
- 47. Full thickness medial collateral ligament rupture.
- 48. Medial collateral ligament injury. Longitudinal scan along the medial aspect of the knee shows thickened medial collateral ligaments with a hypoechoic area denoting acute injury.
- 49. Chronic medial collateral ligament injury with a thickened inhomogeneous ligament intratendinous fissure and neovascularity.
- 50. Lateral collateral ligament injury. Longitudinal scan along the lateral aspect of the knee joint shows a heterogeneous mass replacing the LCL and displacing the biceps tendon anteriorly. The mass represents a hematoma and denotes acute injury.
- 51. Cystic lesions in the medial collateral ligament caused by friction over a bony spur.
- 52. Medial collateral ligament acute tear.
- 53. Ultrasonography of a meniscal tear encompassed a static observation of a hypoechogenic area and a dynamic appreciation of meniscal extrusion. The extrusion of the meniscus when torn depended on a disruption of the ultra structure and hence function of the meniscus. In the presence of a tear the intrinsic stability of the meniscus on loading is lost and this can be detected. The accuracy of ultrasonography by its sensitivity of 86.4%, which matched that of MR scanning, supports its use in the diagnosis of meniscal tears. Given the rapidity with which the investigation can be conducted and the relative lack of expense it is a good investigation for use in a ‘one-stop’ clinic. Before routine use of ultrasonography in the diagnosis of meniscal tears, further improvement is required to address the problem of false-positive results which could lead to inappropriate surgery being performed. The ultrasound to be less specific during the earlier disease stage.
- 54. Meniscal injury. (A) Ultrasound scan along the medial aspect of the knee joint shows a swollen meniscus with a linear hypoechoic cleft denoting meniscal degeneration. (B) Sonogram of the lateral aspect of the knee joint shows a hypoechoic meniscal cyst connected to a meniscal tear.
- 55. Medial meniscal tear: (a) Coronal T1-weighted magnetic resonance imaging, (b) ultrasound
- 57. Horizontal lateral meniscus rupture and meniscal cyst.
- 58. Medial meniscal protrusion and small rupture.
- 59. Meniscal degeneration with protrusion of the lateral meniscus with cysts and bulging of the lateral collateral ligament
- 60. Large medial meniscal cyst and medial meniscal rupture.
- 61. Lateral meniscal cyst extending under the patellar tendon.
- 62. Large cyst at the base of the meniscus in 6 year old child.
- 63. The anterior cruciate ligament (ACL) is an intra-articular structure that originates at the medial wall of the lateral femoral condyle posteriorly and inserts into the intercondylar area of the tibia. The ACL is the primary restraint to anterior displacement of the tibia relative to the femur and acts as a restraint to internal–external rotation. The sonographic appearance of the ACL was a hypoechoic band with a diameter of 7.3 mm. Magnetic resonance imaging (MRI) and sonographic images of the anterior cruciate ligament (ACL) in a normal individual. (A) Sagittal T2- weighted MRI of the right knee with 90° flexion. The decreased T2 signal ACL is within the frame (arrowheads). (B) MRI of the ACL: 135° clockwise rotation and magnification of the frame in (A). (C) Sonographic image of the ACL, showing a hypoechoic band in comparison with the MRI image. Arrowheads = ACL; F = femur; P = patella; T = tibia.
- 64. Arthroscopic and sonographic image of an intact anterior cruciate ligament (ACL). (A) Arthroscopic ACL image. (B) Sonographic image of an intact ACL under arthroscopic guidance. Between the black and white arrowheads is the ACL; white arrow indicates the Kelley. P = patella; T = tibia.
- 65. Magnetic resonance imaging and sonographic images of an individual with a ruptured left anterior cruciate ligament (ACL). (A,B) Magnetic resonance imaging and (C,D) sonographic images of a subject with (A,C) an intact right and (B,D) a ruptured left ACL. (E,F) Dynamic sonographic image of the ACL when individuals rotate their tibia internally or externally.(A) Black arrowheads indicate intact ACL with diameter of 6.4 mm. (B) Black arrow indicates ruptured ACL with a thinner diameter. (C) Between the white arrowheads is the intact ACL appearing as a hypoechoic band. (D) White star indicates ruptured ACL with a heteroechoic appearance. (E) The soft tissue above the ACL moves in the opposite direction to the ACL movement in normal individuals. (F) The soft tissue above the ACL moves in the same direction as the ACL movement in individuals with a torn ACL. F = femur; P = patella; T = tibia.
- 66. The ultrasound role of posterior cruciate ligament injury show all PCLs were hypoechoic , regardless of injury. The injured PCLs had an average diameter of 0.88cm(range 0.54-1.21cm), while the normal PCL had an average diameter of 0.51cm(range 0.30-0.84cm). Focal discontinuity of the ligament is seen in complete ligamentous tear. PCL injury is manifested sonographically either as enlargement of the entire ligament, appreciated by comparison with the contralateral PCL, or by focal disruption of the ligament.
- 67. MR Gradient echo-T2 show abnormal bright signal and the US show Hypoechoic PCL(Arrows).
- 68. MR Gradient echo-T2 show thickened poorly defined PCL and the US show Hypoechoic PCL(Arrows) which appears thickened .
- 69. MR Gradient echo-T2 show thickened distal PCL with abrupt focal cut-off proximally and the US show Hypoechoic PCL(Arrows) with abrupt focal changes in caliber of the ligament.
- 70. A Baker's cyst (also known as a popliteal cyst) is a fluctuant swelling located in the popliteal space. The term is a misnomer as the swelling is the result of synovial fluid distending the gastrocnemius-semimembranosus bursa, rather than being a true cyst. In older patients it is commonly part of a chronic knee joint effusion which herniates between the two heads of the gastrocnemius and is most commonly secondary to degenerative or meniscal pathology. Primary cysts have not been found to communicate directly with the knee joint. These cysts usually occur in young people and are symptomless. Ultrasound scan - differentiates purely cystic masses from more solid lesions and can exclude a DVT. It may also be used to evaluate the cyst's internal structures, exclude other lesions, and assess its relationship to other structures.
- 71. Ganglion cyst on the medial side of the knee.
- 72. Cyst in the retinaculum patellae.
- 73. Baker's cyst. Longitudinal scan of the medial aspect of the popliteal fossa shows a well-defined cystic lesion with a narrow neck. It contains echogenic debris and thick septa, which are characteristics of a complicated Baker cyst.
- 74. Baker's cyst.
- 75. Rheumatoid arthritis: US shows synovial thickening and effusion. The synovial thickening appears hypoechoic or heterogenous proliferation of the synovial membrane with poorly defined contour. Doppler study show increased vascularity within the hypertrophied synovium. Degenerative arthritis: Sonography show extent of cartilage damage and US also show thinning or disappearance of the cartilage. Osteochondral defect of the femoral condyle appears as thinning of the hyaline cartilage or as irregularities or defect of the hyperechoic bone cortex. Bone lesion: The cortex is an intensely hyperechoic interface with distal acoustic shadowing. Fracture appears as breaks or steps in the hyperechoic cortex, often accompanied by a hypoechoic subperiosteal hematoma. Sonography has been used to measure the thickness of the cartilaginous cap of an osteochondroma.
- 76. Rheumatoid arthritis. Longitudinal ultrasound scan shows a small effusion in the suprapatellar bursa with mild irregular thickening of the synovial membrane, which is indicative of inactive disease.
- 77. Degenerative arthritis. Transverse ultrasound scan of the flexed knee shows loss of the normal hypoechoic pattern of the articular cartilage, marked irregularity of the cartilage–soft-tissue interface, and blurring of the bone–cartilage interface.
- 78. Osteochondral defect. Defect and displacement are seen in the hypoechoic articular cartilage and hyperechoic bony cortex.
- 79. Osteochondroma. Ultrasound scan of the knee joint shows bony outgrowth from the upper end of the tibia. Ultrasound can be used to measure the thickness of the hypoechoic cartilaginous cap.
- 80. Loose bodies. Ultrasound scan of the popliteal fossa shows two large loose bodies within a popliteal cyst with posterior acoustic shadowing.
- 81. Soft-tissue masses. (A) Intramuscular ganglion: longitudinal scan along the popliteal fossa shows a well-defined, thick-walled, multiloculated intramuscular cyst with mild flow within the septa with color Duplex examination. (B) Soft-tissue sarcoma: Sonogram shows a large mass in the popliteal fossa with mixed echogenicity and increased vascularity on the color Duplex examination.
- 82. Pigmented Villonodular Synovitis with a vascularized hypoechoic mass on the medial aspect of the knee extending behind the patellar tendon.
- 83. Soft-tissue masses: Ultrasound can differentiate cystic from solid masses, but benign and malignant masses cannot be differentiated. Slandered characteristic such as size, shape, location and the echogenicity can be determined by ultrasound, Color and power Doppler sonography allow assessment of tumour vascularity which is helpful if malignancy is suspected. Hemangiomas have a variable echogenicity with distal shadowing(due to the presence of Phleboliths). Lipoma generally as hyperechogenic masses, Soft tissue sarcomas appear as complex with increased vascularity on color and power duplex sonography. Muscle injury is images with sonography. Focal muscle tears and /or hematomas may appear as simple or complex fluid collection, the age of a hematoma influence is appearance. Rupture of the gastrocnemius is characterized by disruption of the normal parallel , linear echogenic and hypoechogenic appearance of the tendon at its insertion. Fluid collection within the gastrocnemius muscle may be seen. The hemorrhagic fluid is seen as hyperechoic at the early stages.
- 84. Dermatofibroma on the medial side of the knee.
- 85. Gastrocnemius muscle injury. Sonogram of the medial aspect of the popliteal fossa shows disruption of the gastrocnemius muscle with a hyperechogenic intramuscular hematoma denoting acute injury.
- 87. Vascular lesions: Ultrasound can be used to measure an aneurysm of the popliteal artery, Power Doppler sonography can identify the neck of the aneurysm and differentiate between patent and thrombosed parts. Color Duplex ultrasound can be used for detection of deep venous thrombosis within the popliteal vein, which appears distended and non- compressible with an echogenic thrombus, No flow detected within the vein with color Duplex examination.
- 88. Partially thrombosed popliteal artery aneurysm. Color Duplex examination of the popliteal fossa shows color signals within the patent central part of an aneurysm, which is connected to the popliteal artery by a narrow channel. The thrombosed part of the aneurysm shows no flow signal.
- 89. Deep vein thrombosis. Color Duplex examination of the popliteal fossa shows a distended popliteal vein, a thrombus with mixed echogenicity, and no detectable blood flow.
- 90. Thank You.
