Periradicular Surgery: A Concise Guide
- 2. Introduction Over the past decade, periradicular surgery has continued to evolve into a precise, biologically based adjunct to nonsurgical root canal therapy. Although nonsurgical endodontic treatment gives good results in most cases, surgery may be indicated for teeth with persistent periradicular pathoses that have not responded to nonsurgical approaches.
- 3. History Over 1,500 years ago - Aetius, a Greek physician performed first recorded endodontic surgical procedure - incision and drainage of an acute endodontic abscess 5000 BC – Sushruta – performed excision of palatal growth 9th century – Abulcasis – performed surgical removal of epulis and Cautery procedure 1728 - Pierre Fauchard - Replantation and Transplantation techniques 1845 - Hullihen - ‘Hullihen’s surgery’ or ‘Rhizodontrophy’ or Trephination procedure
- 4. History 1871 – Smith - First root end resection 1880 – Brophy - Root end filling 1881 - Claude Martin - Father of root end resection 1884 – Farrar - Root amputation Surgical operating microscopes – - 1980’s - Endodontic microsurgery 1990s – Dr. Gary Carr surgical ultrasonic tips first designed – Carr tips 1999 – Spartan/Obtura - Kim Surgical tips – Kis tips
- 5. Definition A surgical procedure related to problem of the pulp less or periodontallly involved tooth, requiring root amputation and endodontic therapy. (John I Ingle) Removal of tissues other than the contents of the root canal space to retain a tooth with pulpal and/or periapical involvement. (Franklin Weine)
- 6. Rationale To remove the causative agents of periradicular pathology. To restore the periodontium to a state of biologic and functional health.
- 7. Objectives To ensure the placement of a proper seal between the periodontium and the root canal foramina.
- 8. Indications Glick and Ingle 1. Need for surgical drainage Incision and drainage Trephination 2. Failed nonsurgical endodontic treatment Irretrievable root canal filling,material Irretrievable intraradicular post 3. Calcific metamorphosis of the pulp space 4. Procedural errors Instrument fragmentation Non-negotiable ledging Root perforation Symptomatic overfilling 5. Anatomic variations Root dilaceration Apical root fenestration
- 9. 6. Biopsy 7. Corrective surgery Root resorptive defects Root caries Root resection Hemi section Bicuspidization 8. Replacement surgery Replacement surgery Intentional replantation (extraction/replantation) Post-traumatic Implant surgery Endodontic Osseo integrated
- 10. Relative Contraindications 1. Patient’s medical status Major system disorder – Cardiovascular, Respiratory, Digestive, Hepatic, Renal, Immune, Skeleton-muscular 2. Anatomical considerations Nasal floor Maxillary sinus Proximity to neurovascular bundles of mandibular canal and mental foramen limitations to adequate visual and mechanical access 3. Practitioner’s skill and experience
- 12. CLASSIFICATION (by Kim et al) Based on sequence of use: Examination instruments Incision blades Elevation instruments Tissue retraction instruments Curettage instruments Osteotomy instruments Inspection instruments Retro fill carriers Retro fill Pluggers Miscellaneous instruments Suturing instruments Suction tips Irrigation instruments Ultrasonic instruments Surgical operating microscope
- 13. Examination Instruments Dental mirror Periodontal probe Endodontic explorer Micro explorer Tip of microexplorer used to – • Search for leak in root-end filling • Distinguish canal or craze line from microfracture line
- 14. Incision blades Bard Parker Blades: Microblade No. 15c No. 15 No. 12 No. 11 15C blade in use Microblades
- 15. Elevation Instruments Traditional Microsurgical Enlarged tips of soft tissue elevators Molt’s curette (above) Periosteal elevator No. 9 (below)
- 16. Tissue Retraction Instruments Arens tissue retractor Selden retractor University of Minnesota retractor Cats paw retractor
- 17. Curettage Instruments •Minicurettes •Mini jacquette 34/35 •Columbia 13- 14 •Miniendodontic curettes •Minimolten curettes Enlarged tips of minijacquettes and mini- endodontic curettes
- 18. Osteotomy Instruments Straight Handpiece Microhead Handpiece Impact air 45o handpiece with H161 Lindemann bone cutting bur – instrument of choice for osteotomy
- 19. No. 4 round bur No. 6 round bur No. 8 round bur No. 57 fissure bur Multipurpose bur Endo-Z bur
- 20. Inspection Instruments Micro mirrors Round and modified rectangular Flexible neck Stainless steel (top and bottom) Scratch-free sapphire mirror surface (centre two)
- 23. Surgical Operating Microscope Magnification Range = 2X - 32X MAGNIFICATION RANGE Low: 3 - 8 X Medium: 10 – 16 X High: 20 – 30 X The surgical operating microscope was used first time in neurosurgery and ophthalmology in 1960 and Endodontic microsurgeries in 1980s
- 24. Advantages High magnification Surgical technique can be performed precisely and accurately Surgical technique can be easily evaluated Fewer radiographs needed Video recordings possible Reduces occupational stress
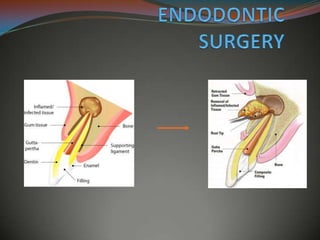
- 25. Classification of Endodontic surgery Fisulative surgery Incision and drainage Cortical trephination Decompression procedures Periradicular surgery Curettage Root-end resection Root-end preparation Root-end filling Corrective surgery Perforation repair Mechanical (iatrogenic) Resorptive Periodontal management Root resection Tooth resection Intentional replantation
- 26. Surgical Drainage : Surgical drainage is indicated when purulent and/or hemorrhagic exudates forms within the soft tissue and the alveolar bone; a result of a symptomatic Periradicular abscess. Surgical drainage maybe accomplished by ; Incision and drainage (I and D) cortical Trephination
- 27. Incision And Drainage Procedure Local anesthetic - Mepivacaine (low pKa) Horizontal incision with No.11 or 12 BP blade at the base of the fluctuant area Frank et al - rubber dam drain to maintain the patency of the surgical opening. McDonald and Hovland - incision alone Gutmann and Harrison- use of drain is Indicated in moderate to severe cellulitis and other positive signs of an aggressive infective process.
- 29. Materials used Iodoform gauze Rubber dam material -“H” or “Christmas tree” shape. Penrose drain Penrose drain Serrated drain
- 31. No 6 or 8 round bur Buccal approach The objective is to create a pathway through the cancellous bone to the vicinity of the involved periradicular tissues. Trephination Cortical trephination is a procedure involving the perforation of the cortical plate to accomplish the release of pressure from the accumulation of exudate within the alveolar bone.
- 33. Treatment planning for periradicular surgery 1. Presurgical patient management 2. Need for profound local anesthesia and hemostasis 3. Management of soft tissue 4. Management of hard tissues 5. Surgical access, both visual and operative 6. Access to root structure 7. Periradicular curettage 8. Root-end resection 9. Root end preparation 10. Root-end restoration 11. Soft-tissue repositioning and suturing 12. Postsurgical care
- 34. PRESURGICAL PATIENT MANAGEMENT Patients medical status Proper history taking is first key for success of any surgical procedure. Patient should be evaluated for major system disorders (cardiovascular, renal, hepatic, digestive, immune and skeletal muscle) which may contraindicate or alter approach to surgery. Also premedication for patient in normal or in presence of any of the above medical conditions should be given priority and consulted with physician.
- 35. Patient preparation Patient preparation starts with patient communication regarding reason for surgery, risks involved, also factors which improve prognosis for successful outcome of surgical procedure. There may be necessity of premedication (sedatives or hypnotics, systemic antibiotics) for patient in order to improve accessibility also postsurgical healing. Presurgical mouth rinse with chlorhexidine gluconate (Peridex) may improve surgical environment by decreasing tissue surface bacterial contamination. Mouth rinse should be started a day before surgery, immediately before surgery, and up to 4 to 5 days post surgically. This reduces bacterial contamination of surgical site and improve wound healing.
- 36. Anaesthesia Local anaesthetic with vasoconstrictor Objectives: obtain profound and prolonged anaesthesia provide good hemostasis both during and after the surgical procedure Selection based on: Medical status of the patient Desired duration of anaesthesia
- 37. TYPES OF LOCAL ANALGESIA Topical analgesia (surface analgesia) Sub mucosal infiltration Sub periosteal infiltration Nerve block analgesia Intra ligamentary analgesia. Intra osseous analgesia. 2 1 3 6 5 4
- 38. TOPICAL ANALGESIA (SURFACE ANALGESIA) An anaesthetic is applied in a gel form to the intact mucous membrane. It passes through the epidermis and makes the nerve endings analgesic prior to administration of a deeper or infiltration analgesic . Use-The surface analgesia prevents the pain of the needle.
- 39. Technique: The mucosa is dried using sterile cotton. A small quantity of local anesthetic paste or ointment is placed on a sterile cotton roll. This is placed on the mucosa at the proposed site for 2 min. Care is taken to prevent its spread elsewhere. Excess is wiped away.
- 40. The solution is deposited around the nerve filaments in the sub mucosa. In supraperiosteal technique, the tip of the needle is placed beneath the sub mucosa in the elastic tissue. The solution does not penetrate the bone. SUBMUCOSAL INFILTRATION
- 41. It should be regarded as a preliminary for depositing sub periosteal LA allowing the placement of the anaesthetic comfortably. It is not useful in simple conservative procedures also . Use-on nervous adults or children where the pressure caused by injecting subperiosteally is too uncomfortable for the patient.
- 42. Technique: Maxillary Maxillary Central Incisor The mucosa is pulled taut and the needle (preferably a short one) is inserted about 8 mm from the gingival margin or about 21 mm from the incisal edge such that the hub of the needle is just apical to the incisal edge. The needle is pushed with a deliberate forward motion. About 1 ml solution is deposited.
- 44. Maxillary Lateral Incisor Shorter root should be considered. Due to palatine position of the apices, often nasopalatine block is required. Maxillary Canine The root is very long 25 mm. Canine eminence to serve as guide.
- 45. Maxillary First Premolar The needle is placed distal to the canine eminence. About 22mm from the buccal cusp. Maxillary Second Premolar The canine eminence and the base of the zygomatic process are used as guide. About 21mm from the buccal cusp. A palatal infiltration is often required for first and rarely second
- 47. Maxillary First /Second/Third Molar Buccal infiltration with a short needle. The presence of zygomatic process makes it necessary for two infiltrations-one mesial to for mesio buccal root (about 23 mm from the MB cusp) and one distal for the disto buccal root (about 21 mm from the DB cusp) The palatal root requires another infiltration about 3- 4mmbeing inserted in into the mucosa about 8 mm from the gingiva.
- 48. Maxillary molars
- 50. Mandibular Central Incisor, Lateral Incisor, Canine The tip of needle is approximately 18 mm from the incisal edge. The needle is placed deep into the sulcus. 0.75-1 ml solution is deposited. A variation is simple infiltration to the interdental papilla. Technique: Mandibular
- 52. Mandibular First /Second Premolar The tip of the needle is close to the root apices in the buccal sulcus .The needle is placed subperiosteally. About 0.5-1ml solution is deposited.
- 54. Mandibular First /Second/Third Molar The tip of the needle is placed in the sulcus adjacent to the apices of the teeth involved. The broad shelf of bone means that it takes a longer time for the penetration of the solution.
- 55. SUBPERIOSTEAL INFILTRATION To ensure adequate anaesthesia it is necessary to insert the needle in the periosteum. The tip of the hypodermic needle is inserted under the periosteum. A lot of pressure must be applied to the plunger to deposit the solution. This can be very uncomfortable and to the patient. painful. Use- Is necessary for conservative procedures.
- 56. NERVE BLOCK ANALGESIA The tip of the hypodermic syringe is inserted near an anatomically discrete nerve bundle and LA is deposited around it. Larger quantity of solution is required. The size of the nerve bundle demands more time for penetration of the solution to the centre The analgesia is profound and extends over the areas served by the nerve bundle.
- 57. Technique: Maxillary Posterior Superior alveolar nerve block First (DB and palatal root) /Second /Third Molar which are supplied by the branches of maxillary nerve through the posterior superior alveolar nerve The needle is inserted distal to the last molar, upwards and medial at about 45°. 1.5 ml of solution on the distobuccal aspect of the maxilla. Complication: vessels of the pterygoid venous plexus are ruptured resulting in haematoma.
- 58. Posterior superior alveolar nerve block
- 59. Middle Superior alveolar nerve block The mesio buccal root of the first molar along with the premolars and the mucosa is supplied by Middle Superior alveolar nerve. 1ml of solution is deposited deep in the sulcus between the second premolar root an d the mesio buccal root of first molar.
- 60. Middle Superior alveolar nerve block
- 61. Anterior Superior alveolar nerve block This nerve supplies the upper canine, lateral incisor and the central incisor.1-1.5 ml of solution to be deposited deep in the sulcus below the level of the infraorbital foramen.
- 62. Infraorbital nerve block Analgesia of the anterior part particularly useful when infection precludes the use of infiltration techniques. The solution is deposited at the entrance of the infraorbital foramen blocking both the ASA and MSA. A swelling of the tissues is felt when the solution is deposited
- 63. The infraorbital ridge is palpated and the notch is identified. The tip of the needle is inserted deep in the sulcus above the apex of the second premolar and advanced till it is 1.5- 2 cm deep.
- 64. Palatine nerve block Analgesia of the palate as far as canine on one side can be achieved by depositing approx 0.5-0.75 ml of solution over the greater palatine nerves as they emerge from the greater palatine foramen. This is distal to the second molar at the junction of the hard palate and the alveolar process. The needle is inserted about 0.5 cm.
- 66. Nasopalatine nerve block The tip is inserted through the nasopalatine papilla until it rests within the entrance to the incisal canal. If the bone is contacted the needle is withdrawn 0.5-1 mm. about 0.1-0.2 of solution is deposited.
- 67. Technique: Mandibular Inferior alveolar nerve block It is the single most important technique in dental practice. Combined with the lingual nerve and the long buccal it provides anaesthesia of hard and soft tissues of one side of the mandible from third molar to incisor
- 68. Considerations A few mm above the occlusal plane in the horizontal section it lies against the medial surface of the ramus in the pterygoid space. Anteriorly- Pterygoid raphe ( buccinators and superior pharyngeal constrictor) Posteriorly –parotid gland. Laterally –medial surface of the ramus. Medially –medial pterygoid muscle.
- 70. When the patient opens his mouth wide it is possible to identify the prominent ridge of pterygo mandibular raphe.
- 71. The thumb is used to retract the cheek and also delineate the apex of the buccal pad of fat. As the thumb is moved backward the external oblique ridge is palpated. The tip of the thumb is moved medially to lie in the retro molar fossa.
- 72. It is then withdrawn slightly and aspirated. 1.5 ml of solution is deposited The needle is then inserted about 0.5 cm and 0.1-0.2 ml solution is deposited to anesthetize the lingual nerve. The needle is then further advanced for 1.5-2 cm until its tip lightly touches the bone.
- 73. Lingual nerve block. It ascends diagonally back through the space until it joins the mandibular nerve superior to the mandibular foramen. A shallow depression above the foramen is the site where the solution is to be deposited. It is achieved by injecting 0.1-0.2 ml of solution at the level of the alveolar crest distal to the second/third molar. It can be done either when the needle is inserted or withdrawn.
- 75. Long buccal nerve block For the analgesia of the mucosa and the gingiva. The needle is inserted distal and buccal to the third molar approx. 1 cm from the distobuccal aspect.0.5 ml solution is deposited.
- 76. Mental nerve block Solution deposited at the level of mental foramen enters reaches the inferior alveolar nerve to anesthetize the premolars, canine and incisors of that side. 1.5-2 ml solution is deposited deep in the sulcus.
- 77. INTRALIGEMENTARY ANALGESIA The tip of 30 gauge needle is inserted into the coronal part of the periodontal ligament and solution is injected under high pressure. Use- This provides anaesthesia to a single tooth.
- 78. Shapes of the syringes are modified to achieve high pressure. The 30 gauge needle is inserted through the gingival sulcus into the periodontal ligament. The needle is angled about 30° to the long axis of the tooth. The needle is pushed approx. 2 mm into the periodontal ligament parallel to the root surface. Continuous and firm pressure is applied for 20-30 sec. An strong resistance is felt. About 0.05-0.1 ml solution is deposited. This is done at all four corners of the tooth .Max of 0.4-0.8 ml of solution is injected .The needle is then held for 5-10 sec to dissipate the pressure before needle is withdrawn.
- 82. INTRA OSSEOUS ANALGESIA A small hole is drilled through the mucosa and the bony cortex to allow the insertion of a needle directly into the bony medulla enabling profound analgesia around a group of teeth. There is a high risk of the solution to be taken up in the blood stream. Use- only when other techniques have failed.
- 83. A sterile 1 or 2 round bur assisted by copious supply of water is used to drill through the mucosa .the cortical bone and medullary bone. The needle is inserted into the bony medulla and 1-2 ml of solution is deposited at the apex of the tooth. Dis: Local anesthesia is deposited very near vascular area and the levels of LA increase dramatically.
- 84. LOCAL COMPLICATIONS Failure to obtain analgesia Usually due to faulty technique. Presence of infection Best to repeat the procedure. Particular attention to the anatomical landmarks. LA should be given in a remote area. Nerve block anaesthesia is important.
- 85. Pain during injection Poor technique Good technique as well as gentle and slow injection should be followed. Warming the anaesthetic syringe just before injecting reduces discomfort. Rarely a sharp electric shock is felt along the nerve. This indicates nerve sheath being pierced. Needle should be withdrawn.
- 86. Haematoma formation In areas of great vasculature ,blood vessels may be punctured. This results in bleeding in the tissues with a haematoma being developed. The patient should be reassured that the haematoma will dissipate over a week or 10 days like a bruise. Antibiotic therapy should be started as there are chances of infection.
- 87. Intra vascular injection This can be prevented by using a aspirating syringe Trismus Muscle spasm which makes it difficult to open mouth. Results when an injection into the medial pterygoid causes a tearing of the muscle fibers and a haematoma. Onset is more than 24 hours later.
- 88. Blanching Which occurs at the site of injection : Due to combined defect of the hydrostatic pressure of the local anaesthetic and the vasoconstrictor. Which occurs at a remote site : Either due to an inadvertent intravascular injection or interference with the autonomic nerve supply of the blood vessels affected by the local anaesthetic.
- 89. Blanching covers a variable area of the face and lasts from 30 seconds to 30 minutes after it disappears without any trace .No treatment is required.
- 90. Paralysis Unilateral paralysis of the facial muscles is an uncommon complication and when it does happen it is due to inferior alveolar nerve. It occurs because the tip of the needle is positioned too far back in relation to the mandible and enters the parotid gland where it makes the branches of facial nerve analgesic.
- 91. The complication is alarming to the patient. Dental treatment should be abandoned. The patient should be reassured. The patient should be advised to protect the conjunctiva and avoid scratching of eyelid
- 92. Prolonged impairment of the sensation This is caused by direct damage from the needle or due to small haematoma. The patient should be monitored at regular intervals and the paraesthesia should be mapped by tests. Recovery should be complete within 3 months.
- 93. Lip Trauma Usually occurs in children who had an inferior nerve block. As sensation start to return but while the lip is still numb and rubbery children are inclined to bite their lip to test its feeling unaware that this can cause severe trauma. Untreated a bite can develop a fibrin slough.
- 94. Prevention being better than cure. The parents should be advised to discourage the child. The wound should be kept moist by smearing a thin layer of sterile Vaseline over it every few hours. The traumatic ulcer usually heals without
- 95. Visual disturbances Due to vascular spasm or intra-arterial injection. Normal vision usually returns after 30 minutes. The patient should be reassured but not discharged until vision returns.
- 96. SYSTEMIC COMPLICATIONS Vasovagal attack The most frequently encountered complication. Emotional disturbance leading up to the administration of LA predisposes to a faint. The patient tends to tense himself up to cope with the injection. Immediately afterwards the strain of his exertions seems to overwhelm him-with the massive vagal discharge plus the arteriolar dilatation leading to a reduction in the blood returning to the heart, which in turn results in a gross reduction in cardiac output .
- 97. The consequence is a sudden loss of consciousness, the patient collapses within a few seconds. The patient becomes pale, suffers nausea and dizziness and out in a cold sweat. His skin feels cold and clammy and further he will lose consciousness and pupils dilate. Pulse becomes weak and thready and may in a short while appear t be absent. The patient should be placed in a supine position and a head low position. this encourages the return of blood to the heart which in turn will stimulate cardiac output.
- 98. The airway should be checked ,the jaws should be drawn forward. Any tight clothing should be loosened. Patients usually respond in 2-3 minutes. A few remain confused over some time An apparent simple faint represents a severe disturbance of the cardiovascular and the central nervous systems and should not be taken lightly. Unless it is essential to complete the dental treatment on the same day ,the patient should be appointed on next day.
- 99. Systemic toxicity Despite the fact that LA solution are injected in a very vascular area toxic reactions are rare. When they do occur there may be convulsions, respiratory depression, or even circulatory collapse .These symptoms pas relatively early. Indeed they may be of such short duration that they may not be observed.
- 100. Drug interactions This is a potential problem when the patient is taking systemic medications. The LA containing noradrenaline can potentiate the blood pressure response in patients receiving tricyclic antidepressants.
- 101. Allergy A patient may report to the dentist stating that he is allergic to LA. This should be confirmed by a subcutaneous injection If there is an erythema the cause should be determined , methyl paraben (preservative ) is the cause.
- 102. Idiosyncracy This is a systemic complication that results in an individualized reaction in the patient. Psychogenic factors play an important role. Toxic symptoms are seen even when the dose is below maximum. May lead to serious reaction.
- 103. Homeostasis Adequate homeostasis is a pre requisite for endodontic surgery 1. Mechanical agents: Bone wax 2. Chemical agents a. Vasoconstrictors b. Ferric sulfate 3. Biologic agents : Thrombin 4. Resorbable hemostatic agents i. Calcium sulfate ii. Gel foam iii. Absorbable collagen iv. Microfibrillar collagen hemostats v. Surgicel (Kim & Rethnam: DCNA; 41; 1997)
- 104. Treatment planning for periradicular surgery 1. Presurgical patient management 2. Need for profound local anesthesia and hemostasis 3. Management of soft tissue 4. Management of hard tissues 5. Surgical access, both visual and operative 6. Access to root structure 7. Periradicular curettage 8. Root-end resection 9. Root end preparation 10. Root-end restoration 11. Soft-tissue repositioning and suturing 12. Postsurgical care
- 105. Management of soft tissue PRINCIPLES OF FLAP DESIGN 1. Making sure base of the flap should be wider than the free end. 2. Avoiding the incision over a bony defect 3. Including the full extent of the lesion. 4. Avoiding sharp corners 5. Avoiding incision across a bony eminence
- 106. 6. Avoiding incision in the mucogingival junction. 7. Taking care during retraction. 8. Incision should be made with firm, continuous firm stroke perpendicular to the cortical bone plate. 9. The sutured flap margin should rest on solid cortical bone plate.
- 107. Classification Full thickness (Mucoperiosteal) - Epithelium + Connective tissue + Periosteum Partial thickness (Split) - Epithelium + Connective tissue According to Gutmann & Harrison Full mucoperiosteal Limited mucoperiosteal Full mucoperiosteal flap – no attached Gingiva around neck of crown Limited mucoperiosteal showing - Remaining attached gingiva
- 108. Full mucoperiosteal flap Triangular Rectangular Trapezoidal Horizontal/Envelope Papilla base Limited mucoperiosteal Sub marginal curved/Semilunar Sub marginal scalloped rectangular/Luebke Ochsenbein
- 109. Advantages of Full Mucoperiosteal Flaps 1. Rapid wound healing 2. Good surgical access 3. Minimal disruption of blood supply 4. Minimal untoward post-surgical sequelae 5. Optimal apical orientation and 6. Primary intentional healing. Disadvantages 1. Loss of soft tissue attachment 2. Loss of crestal bone height 3. Post surgical flap dislodgement
- 110. Advantages of limited mucoperiosteal flap 1. Marginal and interdental gingiva not involved 2. Unaltered soft tissue attachment level 3. Crestal bone is not exposed 4. Adequate surgical access and 5. Good would healing potential Disadvantages 1. Disruption of blood supply to unflapped tissues 2. Flap shrinkage 3. Difficult flap re-approximation 4. Delayed secondary wound healing. 5. Limited apical orientation
- 111. TRIANGULAR FLAP INDICATIONS: Mid root perforation repair Periapical surgery in posterior areas with short roots ADVANTAGES: ○ Good wound healing ○ Minimal disruption of vascular supply to flapped tissue ○ Ease of flap re-approximation with minimum number of sutures DISADVANTAGES: ○ Limited surgical access ○ Difficult to expose the root apices of long teeth like maxillary and mandibular canines ○ Tension is created on retraction
- 113. RECTANGULAR FLAP INDICATIONS: Mandibular anteriors Multiple teeth Teeth with long roots like maxillary canines ADVANTAGES: Increased surgical access to root apex Reduces retraction tension DISADVANTAGES: Difficulty in re-approximation of flap margins Post surgical stabilization is difficult Gingival attachment violated, gingival recession, crestal bone loss may occur
- 115. TRAPEZOIDAL FLAP Similar to rectangular except the 2 vertical incisions intersect the horizontal incision at an obtuse angle → to create a broad based flap with the vestibular part wider than the sulcular portion Disadvantages: Angled incision – severs more vital structures More bleeding Disruption of vascular supply to non-flapped tissues Shrinkage of flapped tissues
- 116. HORIZONTAL FLAP Horizontal intrasulcular incision with no vertical releasing incision Limited applications - Limited access Repair of cervical defects (root perforations, resorption, caries) Hemi sections and Root amputation ADVANTAGES: Ease of repositioning as no vertical incision DISADVANTAGES: Limited access and visibility Difficult to reflect and retract Predisposed to stretching and tearing
- 117. SUBMARGINAL CURVED/SEMILUNAR FLAP INDICATION 1. Esthetic crowns present 2. Trephination ADVANTAGES Reduces incision and reflection time Maintain integrity of gingival attachment Eliminates potential crestal bone loss DISADVANTAGES Limited access and visibility Tendency for increase hemorrhage Crosses root eminences May not include entire lesion Predisposed to stretching and tearing Repositioning is difficult Healing is associated with scar
- 118. SUBMARGINAL SCALLOPED RECTANGULAR/ LUEBKE OCHSENBEIN FLAP Modification of rectangular flap Horizontal incision is placed in buccal/labial attached gingiva & is scalloped - follows the contour of marginal gingiva INDICATIONS Prosthetic crowns Periradicular surgery of anterior region longer roots
- 119. ADVANTAGES Ease in incision and reflection Enhanced visibility and access Ease in repositioning Maintains integrity of attachment Prevent gingival recession Avoid dehiscence Prevent crestal bone loss DISADVANTAGE Horizontal component disrupts blood supply Vertical components crosses mucogingival junction and may enter muscle tissue Difficult to alter if size of lesion misjudged
- 120. INCISION Incisions for the majority of mucoperiosteal flaps for periradicular surgery can be accomplished by ; No.11, NO.12, No.15, No.15C, micro surgical blade.
- 121. FLAP REFLECTION Flap reflection is the process of separating the soft tissue (Gingiva Mucosa and Periosteum) from the surface of the alveolar bone. This process should begin in the vertical incision a few millimeter apical to the junction of the horizontal and vertical incisions. Periosteal elevator for flap reflection are ; No.1 and No.2 (Thompson Dental Manufacturing Co) No.2 (Union Bronch) No.9 (Union Bronch Co)
- 122. FLAP RETRACTION Process of holding in position the reflected soft tissues Provides visual and operative access Tissue retractor must always rest on solid cortical bone with firm light pressure
- 123. HARD TISSUE MANAGEMENT Osteotomy Following reflection and retraction of the mucoperiosteal flap, surgical access must be made through the cortical bone to the roots of the teeth. Methods to locate the root apex Methylene blue dye Visual and tactile method(Barnes) 1. Root structure generally has a yellowish color 2. Roots does not bleed when probed 3. Root texture in smooth and hard as opposed to the granular and porous nature of bone 4. The root is surrounded by the PDL
- 124. OPTIMAL OSTEOTOMY SIZE Traditional endodontic surgery - approximately 10 mm in diameter. Should be just large enough to manipulate ultrasonic tips freely within the bone crypt. Since the length of an ultrasonic tip is 3 mm, the ideal diameter of an osteotomy is about 4mm.
- 125. Periradicular curettage A surgical procedure to remove diseased or reactive tissue from alveolar bone in the periradicular area or lateral region surrounding a pulp less tooth (AAE 1994) Purpose: • To remove pathological periradicular tissues for visibility and accessibility for treatment of apical root canal system • To remove foreign material present in periradicular tissues
- 126. To accomplish removal of entire mass, the largest bone curette, consistent with the size of the lesion, is placed between the soft tissue mass and lateral wall of the bony crypt with concave surface of curette facing the bone. Once soft tissue has been freed along the periphery of the lesion, the bone curette should be turned with concave portion towards the soft tissue and used in scraping fashion to free tissue from deep walls of bony crypt.
- 127. Root End Resection Indications Eliminating Anatomical variations Ledges Canal obstructions Resorptive defects Perforation defects Separated instruments Visualize seal created by orthograde treatment and need for root- end seal Gain access to pathological tissue trapped along lingual surface of root
- 128. Ingle et al recommended the root end resection is best accomplished by the No.702 tapered fissure bur or No.6 or No.8 round bur in a low speed straight hand piece. Lasers Komori and associates evaluated the use of the Er:YAG laser for root-end resections: Er:YAG laser - smooth, clean, resected root surfaces free of any signs of thermal damage. INSTRUMENTS
- 129. Moritz and associates CO2 laser treatment optimally prepares the resected root-end surface to receive a root-end filling seals the dentinal tubules eliminates niches for bacterial growth sterilizes the root surface Advantages of the laser use: Absence of discomfort and vibrations Less chance for contamination of the surgical site Reduced risk of trauma to adjacent tissue
- 130. Rationale for laser use in endodontic periradicular surgery includes (Miserendino et al) (1) improved homeostasis and concurrent visualization of the operative field (2) potential sterilization of the contaminated root apex (3) potential reduction in permeability of root-surface dentin (4) reduction of post-operative pain (5) reduced risk of contamination of the surgical site through elimination of the use of aerosol-producing air turbine hand pieces.
- 131. EXTENT OF APICAL RESECTION
- 132. BEVEL ANGLE Historically – 30-45o: to gain visual and operating access to the root tip for resection, placement of retro filling materials, and inspection. Present - 90o Maximum= 10o degree bevel Advantages: •Exposes fewer dentinal tubules, thus preventing excess leakage and contamination.
- 133. ROOT END PREPARATION Purpose: • To create a cavity to receive a root-end filling. Objective: It must be placed parallel to the long axis of the root. Instruments Used: Small round or inverted cone burs Ultrasonic tips
- 134. IDEAL ROOT END PREPARATION The apical 3 mm of the root canal must be freshly cleaned and shaped. The preparation must be parallel to and coincident with the anatomic outline of the pulp space. Adequate retention form must be created. All isthmus tissue, when present, must be removed. Remaining dentin walls must not be weakened.
- 135. Traditional root-end cavity preparation technique Miniature contra-angle or straight hand piece Small round or inverted cone bur. Class I cavity preparation along the long axis of the root within the confines of the root canal. Recommended depth - 2 to 3 mm being the most commonly advocated. (Gutmann and Harrison) Disadvantage: Apical perforation due to difficulty in aligning the bur
- 136. Recently, specially designed ultrasonic root end preparation instruments have been developed. Ultrasonic tips developed by De Gary Carr- Available with plain and diamond coated tips. Kis Microsurgical Ultrasonic Instruments – The tips are coated with zirconium nitrite for faster dentin cutting with less ultrasonic energy
- 137. Advantages of Ultrasonic tips over micro head burs Need for beveling eliminated Tip stays centered in root and follows canal space ↓ chances of lingual or lateral root perforations Conserving greater thickness of root canal wall Better access to surgical areas, especially difficult to reach areas such as lingual apices Deeper root-end preparation achieved
- 138. Less dentinal tubules exposed Cleaner cavity than bur – smoother, less debris and smear layer Ultra precise isthmus preparations. Parallel canal walls preparation for better retention of filling materials. Drawbacks: Creation of micro cracks due to vibrations produced
- 139. RETROGRADE RESTORATIVE MATERIALS AND TECHNIQUES Purpose: To seal the apex so that no bacteria or bacterial by products can enter or leave from the canal Properties of ideal retrograde restorative materials : Well tolerated by periapical tissues Bactericidal or bacteriostatic Adhere to the tooth Dimensionally stable Readily available and easy to handle
- 140. Not stain teeth or periradicular tissue Non corrosive Resistant to dissolution Electrochemically inactive Promote Cementogenesis Radiopaque
- 141. Root End filing materials : Gutta percha Amalgam Cavit IRM Super EBA Glass Ionomer Composite resins Carboxylate cements Zinc phosphate cements Zinc oxide eugenol cements Mineral trioxide aggregation (MTA)
- 142. The prognosis ultimately depends on factors such as: An accurate bevel Adequate access Homeostasis Accurate retrograde preparation Accurate retrograde restoration Existent periodontal disease Occlusal trauma Missed vertical fractures Quality of the orthograde filling Individuals host response.
- 143. SOFT TISSUE REPOSITIONING AND COMPRESSION The elevated muco periosteum gently replaced to its original position with the incision lines approximated as closely as possible. Type of flap design will affect the ease of repositioning. Tissue compression: Using a surgical gauze moistened with sterile saline, gently apply firm pressure to the flapped tissue for 2 to 3 minutes (5 minutes for palatal tissue) before suturing. Enhances intravascular clotting in the severed blood vessels
- 144. SUTURING Purpose: To approximate the incised tissue and stabilize the flapped muco periosteum until reattachment occurs. CLASSIFICATION OF SUTURE MATERIALS Based on material: Synthetic fibers Natural Nylon Collagen Polyester Gut Polyglactin Silk Polyglycolic acid Absorbency: Absorbable Non absorbable Polyester Silk Polyglactin Nylon Polyglycolic acid Collagen Gut
- 145. Size: USP size: 3-0, 4-0, 5-0, 6-0. The higher the first number, the smaller the diameter of the suture material. Structure: Monofilament and Multi filament Twisted and Braided
- 146. Silk Sutures: Non absorbable, multi filamentous, and braided. High capillary effect Enhances movement of fluids and microorganisms between fibers Plaque accumulation on the fibers Severe oral tissue reactions Prevented by postoperative rinse with chlorhexidine Advantage: Ease of manipulation
- 147. Gut: Collagen is the basic component of plain gut suture material derived from sheep or bovine intestines. The collagen is treated with diluted formaldehyde to increase its strength Shaped into the appropriate monofilament size. Gut sutures are absorbable in 10 days Chromic gut: plain gut treated with chromium trioxide. delayed absorption rate Gut suture material is available in sterile packets containing isopropyl alcohol.
- 148. Polyglycolic Acid (PGA): made from fibers of polymerized glycolic acid - absorbable. The rate of absorption is about 16 to 20 days. Multi-filament, braided and handling characteristics similar to silk. First synthetic absorbable suture and it is manufactured as Dexon. Polyglactin (PG): Developed by Craig and coworkers In 1975 Copolymer of lactic acid and glycolic acid Called polyglactin 910 (90 parts glycolic acid and 10 parts lactic acid). Sutures of polyglactin are absorbable, braided and multi filament. Commercially available as Vicryl
- 149. NEEDLES Needle with reverse cutting edge (the cutting edge is on the outside of the curve) is preferable. Available in arcs of 1/4, 3/8, 1/2 and 5/8 of a circle, with the most useful being the 3/8 and 1/2 circle.
- 150. SINGLE INTERRUPTED SUTURE SUTURING TECHNIQUES
- 151. INTERRUPTED LOOP (INTERDENTAL) SUTURE
- 152. POST OPERATIVE INSTRUCTIONS AND CARE Do not lift up lip or pull back the cheek to look at where the surgery was done. A little bleeding from surgical is normal. This should only last for a few hours. A little swelling and bruising face may be evident which may last for a few days. Do not drink alcohol or use tobacco (smoke or chew) for the next 3 days. Have a good, soft diet and drink lots of liquids for the first few days after surgery.
- 153. Place an ice bag (cold) on face where the surgery was done. Leave it on for 20 minutes and take it off for 20 minutes. Continue this for 6 to 8 hours. Take the prescribed medicines as recommended. Rinse the mouth with 1 tablespoon of the chlorhexidine mouthwash twice daily for 5 days. Suture removal after 5-7 days by the dental personnel only. Maintain post operative follow up recall visits If any problems exists inform and visit your dentist immediately.
- 154. BARRIER MEMBRANE TECHNIQUES IN ENDODONTIC SURGERY Regeneration: is the replacement of destroyed tissue with new tissue formed by the cells of the same origin. This new tissue reacts in a similar manner against pathologic stimuli as the original tissues. Repair: is the restoration of the destroyed tissue by disease with new tissue consisting of cells different from the original cells. These cells react differently from the original cells against pathologic stimuli.
- 155. Materials used: GTR membrane Calcium sulphate Periosteal graft Platelet rich plasma Tri calcium phosphate Objective: To enhance the quality and quantity of bone regeneration in the peripheral region and to accelerate bone growth in circumscribed bone cavities after endodontic surgery.
- 156. GTR Membrane Indication Through and through periapical lesion. Large periapical lesion Endo-perio lesion Periapical lesion communicating with the alveolar crest Furcation involvement as a result of perforation Root perforation with bone loss to alveolar crest
- 157. Advantages: ○ Barrier function in case of lack of periosteum. ○ Greater concentration of osteogenic cells in the healing area ○ High success rate. Disadvantages: ○ Cost ○ Possibility of infection ○ Need for a second surgery (non resorbable materials only) ○ Need for a space-maintaining device in large defects ○ Problems in the application of the barrier. ○ Operator skill (e.g. , high surgical skill required when a palatal flap is raised)
- 158. CALCIUM SULFATE Indications : Post apicoectomy bone defects Through and through lesions Periapical lesions with furcation involvement Post surgical endo-perio communications. Advantages: Inexpensive No inflammatory reaction Absence of post operative complications. Possibility of using the materials even in a septic environment Ability to achieve secondary closure of soft tissue on the exposed material. Stabilization of blood clot. Adhesion to root surface. Biocompatible Complete absorption.
- 159. Actions: 1. Periosteum Osteo progenitor cells Osteogenesis 2.Barrier for epithelial infiltration Indications: multifaceted endodontic- periodontic problems Advantages: ○ Highly vascular ○ Easily harvested ○ Configuration adjusted to shape of recipient site Disadvantages: ○ Profuse bleeding ○ Difficulty in obtaining the split thickness graft PERIOSTEAL GRAFT AS BARRIER MATERIAL: (Kwan et al 1998)
- 160. Platelet rich plasma – Rich source of growth factors Properties and Advantages: •Decreased intra operative and post operative bleeding •Rapid soft tissue healing •Rapid vascularization •Decreased post operative pain •Osteo conductive •Hemostatic properties •Safe •Affordable (Demiral et al JOE , 30 (11) , 2004) PLATELET RICH PLASMA + TRI CALCIUM PHOSPHATE
- 161. Corrective surgery Corrective surgery is categorized as surgery involving the correction of defects in the body of the root other than the apex. Corrective surgical procedure may be necessary as a result of procedural accidents, resorption (internal or external), root caries, root fracture, periodontal disease. Corrective surgery may involve Root resection. Hemi section. Intentional replantation.
- 162. ROOT AMPUTATION Root amputation procedures are a logical way to eliminate a weak, diseased root to allow the stronger root(s) to survive when, if retained together, they would collectively fail.
- 163. Distance between pulp chamber floor and coronal aspect of the root separation= 3mm (Minimum) 2 mm allow for establishment of supra crestal attachment apparatus and 1 mm for placement of crown margins
- 164. INDICATIONS FOR ROOT AMPUTATION: (Rosenberg et al) Existence of periodontal bone loss to the extent that periodontal therapy and patient maintenance do not sufficiently improve the condition. Destruction of a root through resorptive processes, caries, or mechanical perforations. Surgically inoperable roots that are calcified, contain separated instruments, or are grossly curved. The fracture of one root that does not involve the other. Conditions that indicate the surgery will be technically feasible to perform and the prognosis is reasonable.
- 165. CONTRAINDICATIONS FOR ROOT AMPUTATIONS: Lack of necessary osseous support for the remaining root or roots. Fused roots or roots in unfavorable proximity to each other. Remaining root or roots endodontically inoperable. Lack of patient motivation to properly perform home-care procedures.
- 166. HEMISECTION Hemi section is defined as separation of a multi rooted tooth and the removal of a root and the associated portion of the clinical crown. Sutures placedResected root Deep periodontal pocket Flap raised
- 167. BISECTION OR “BICUSPIDIZATION” Refers to a division of a crown that leave the two halves and the respective roots. BS should be considered in mandibular molars in which periodontal disease has invaded the bifurcation and repair of internal furcation perforation has been unsuccessful. The furcation is then turned into an interproximal space where the tissue is more manageable by the patient
- 168. BICUSPIDIZATION
- 169. INTENTIONAL REPLANTATION Defined as the act of deliberately removing a tooth and following examination, diagnosis, endodontic manipulation and repair returning the tooth into its original socket. INDICATIONS Difficult access Anatomic limitations Perforation in areas not accessible surgically. Failed apical surgery Apical surgery creating defect Accidental avulsion( unintentional replantation)
- 170. Contraindication Pre-existing moderate to severe periodontal disease Curved and flared roots Non restorable tooth Missing interseptal bone 3 factors that directly affect the outcome of intentional replantation. Extra oral time Keeping PDL cells viable Minimizing damage to the cementum and pdl ligament cells during elevation and extraction
- 171. Endodontic microsurgery DEFINITION A surgical procedure on exceptionally small and complex structures with an operation microscope. (Kim et al) The microscope has changed surgical endodontics from a “blind” technique to one that is visually dominated. It enables the surgeon to assess pathological changes more precisely and to remove pathological lesions with far greater precision, thus minimizing tissue damage during surgery.
- 172. Indications Failure of previous nonsurgical endodontic treatment Failure of previous endodontic surgery Anatomic deviation Procedural errors Contraindication Periodontal health of the tooth Patient health consideration Surgeons skill and ability Hard tissue management Osteotomy: H161 lindermann bone cutter----- 8x to 16x Periradicular curettage: Columbia no 13 and no14 ---10x to 16x Apical resection: lindermann bur -----4xto 8x
- 173. Comparison of traditional v/s microsurgery Kim and Rubenstein, 2001 PROCEDURE TRADITIONAL MICRO-SURGERY Identification of apex Difficult Precise Osteotomy Large (=>10 mm) Small (<5mm) Root surface inspection None Always Bevel angle Large (45o) Small (<10o) Isthmus identification Nearly impossible Easy Retro preparation Approximate Precise Root end filling Imprecise Precise
- 174. SURGICAL SEQUELAE Pain: - Minimal and of short duration, if the tissue management is adequate - Long acting Local anesthetics - Analgesics and Anti inflammatory drugs Swelling: Causes: ○ Post surgical edema ○ Hematoma ○ Infection Management: Inform patient Reassure patient Cold pack application
- 175. MANAGEMENT: Cold pack application Pressure packs: 2X 2 inch gauge or wet tea bag held with moderate pressure for 10- 15 minutes. If severe return to the dental clinic - Resuturing and use of hemostatics (Tannic acid: hemostatic) •Improper elevation and Retraction •Incision into muscle attachment •Inadequate suturing •Trauma due to brushing, mastication Bleeding
- 176. Common in elderly patients with fragile capillaries Causes: •Bruising •Soft tissue compression Depends on: site degree of trauma complexion Ecchymosis Discoloration of the facial or oral soft tissues caused by extravasation and subsequent breakdown in the subcutaneous tissue
- 177. CONCLUSION Endodontic surgery is dynamic and it is imperative that scientific investigation continue, concepts ,techniques and materials used in endodontic surgery must be continually evaluated and modified and more emphasis must be placed on the assessment of long-term outcome
- 178. REFERENCE Pathways of the Pulp by Stephen Cohen, Richard C. Burns,7th,8th Edition Endodontics by John I. Ingle, Leif Bakland 5th Edition Microsurgery in Endodontics: Syngkuc Kim Surgical Endodontics: Guttman and Harrison: Mosby:1994. Contemporary surgical endodontics: Stockdale: 2 Edition Contemporary oral and maxillo facial surgery:Peterson: 5th Edition. Colour Atlas of surgical endodontics: Barnes Colour atlas of endodontic surgery: Loushine Microscopes in endodontics: DCNA: Syngkuc Kim, July; 41 (3)1997. Ultrasound real time imaging in the differential diagnosis of periapical lesions: Cotti et al. IEJ; 36; 2003.
